this post was submitted on 27 Dec 2023
1133 points (98.8% liked)
People Twitter
5974 readers
1801 users here now
People tweeting stuff. We allow tweets from anyone.
RULES:
- Mark NSFW content.
- No doxxing people.
- Must be a pic of the tweet or similar. No direct links to the tweet.
- No bullying or international politcs
- Be excellent to each other.
- Provide an archived link to the tweet (or similar) being shown if it's a major figure or a politician.
founded 2 years ago
MODERATORS
you are viewing a single comment's thread
view the rest of the comments
view the rest of the comments
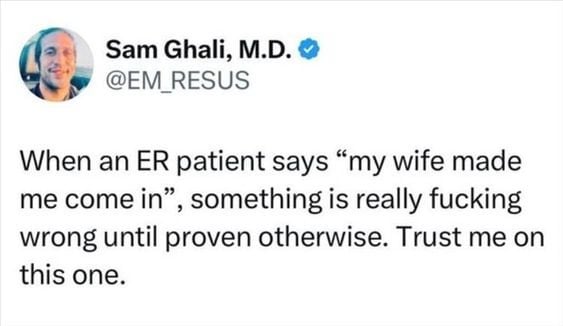
For anyone doubting these experiences, I am a US medical student, and implicit biases and racism are big topics we are taught and made aware of due to physicians profiling their patient whether intentionally or not.
This is especially common in the ER where many people without PCPs come in for issues that are generally handled by a PCP. One of the more difficult things that physicians struggle with is balancing time with the quality of care they provide to their patients. Profiling makes the "time" component easy, but obviously that results in very poor quality healthcare.
No one should be doubting people's experiences of racism and discrimination in the ER and beyond. Doctors are people too, and the bigoted behavior you see in other professions are just as likely to appear with your doctor.
It's nice to see that someone is going to be one of the good doctors.
I appreciate that, and I want to offer hopefully a more positive outlook. These topics are becoming standard courses in the US medical school curriculum, as in they have to be taught to medical students.
It won't solve every problem, of course, but the curriculum is way more patient-oriented than it used to be instead of being a simple "solve disease" kind of curriculum, which is what most of the doctors you see today are taught with.
I rarely comment on lemmy, but I had to say something against the few people who were saying these experiences aren't valid.
Discrimination is real, and don't assume Doctors are perfect because they're not. Of course be open-minded and don't be antagonistic to the ones who are legitimately trying to help you, but if you feel your care wasn't great, then that's very likely a failure on the physician's part.
That is really good news that it's becoming standard. I sincerely hope the grueling hours don't take its toll on you and that they're working on that as well. Burnt out doctors shouldn't be a thing.
I'm a medical student that is aiming for emergency medicine, and threads like these are a special kind of demoralizing. When I was working as an ER tech, there were a fair few times where aggressive or combative patients would only let me get anywhere near them for anything because I never showed any judgement or disdain. Not that I blame my coworkers. It's hard to treat someone nicely after they fake having an overdose in the lobby and then assault one of the nurses after they "wake up" from the narcan.
I honestly think that most medical workers are a victim of the healthcare system and pharma drug pushing as much as the patients. If there was affordable healthcare and a focus on helping people live healthy lives, there wouldn't be so much drama and life threatening decisions.
I know that the general public's idea of what ERs are for doesn't help. EMTALA doesn't mean that everyone who comes into an ER will get treated for anything regardless of ability to pay. It's that they'll be treated and stabilized for any emergent medical condition, illness, or injury... And many people seem to have interesting ideas about what constitutes an "emergency".
The presumption that every patient is someone who fakes an overdose until proven otherwise is precisely why so many people in this threat is suffering. We aren't asking you to serve narcan on a silver platter to people who fakes an overdose. We're just asking to be treated as humans, with empathy, without preconceptions about who we are or why we are at the ER based on our skin color, sex, age, and chronic medical conditions.
Trust us, we know what it's like to feel demoralized at the ER. I've had enough close calls of neglecting life threatening conditions, enough of ER staff laughing off my pain, enough ER staff deliberately manhandling me and hurting my tender points to prove I'm 'overreacting', enough of waiting 6 hours only to be sent home with nothing and in more pain than I was to begin with, enough of being left to cry in pain for hours at the ER and being ridiculed for it. Many of us are demoralized to the point of fearing the ER and avoiding it even under life threatening circumstances, because going through another ER experience might be the tipping point to actually kill ourselves.
There is only so much suffering, pain, and psychological torture the human mind can endure. Most people in the ER have no idea how much chronic pain sufferers have at stake when going to the ER. I have had ER visits that left me more broken than being sexually assaulted as a teen. I trusted doctors, I trusted the hospital, and I trusted that I was in a safe space. Being painfully jabbed, mocked, laughed at, and told im lying and drug seeking were the last things I was expecting. Nothing will repair this breach of trust, because the stakes are too high. I cannot gamble away my physical and mental health for the sake of improving moral in ER staff. For you, at worse you become disillusioned with your career. For me, it's my life that I'm risking.
He came in for an entirely unrelated complaint and faked the overdose to get taken back immediately. The only drug in his system at the time was meth. Literally every room was full except for the resuscitation bay where we took him, and we had to keep him there for almost 2 hours until we had somewhere to move him to. It was the biggest of the resuscitation bays we had, so if we had someone coming in that needed ECMO, we'd have been kind of fucked.
I wish we hadn't had to deal with that guy. Every nurse in the department had minimum 5 patients, mostly high acuity, and his stunt backed up the department for an extra couple hours by pulling unnecessary attention. I much rather would have been helping the nice gentleman in the lobby who had been waiting 5 hours with chest pain and a cardiac history, or the sickle cell patient in pain crisis.
I don't have a problem with drug seeking. Pain is horrible and substance use disorders are diseases, not moral failings. I do have a problem with attention seeking, malingering, and abuse or assault of staff. As a physician, I plan to treat pain appropriately with the necessary medications or therapies, and to treat abuse of my staff with extreme prejudice.
And an edit to add: a drug overdose is treated as the same level of emergency as a cardiac arrest. We don't serve Narcan on a silver platter, we serve it via wide bore IV while getting set up for intubation and resuscitation if it fails because we mean to move heaven and earth to keep the patient alive. An OD gets you to the front of the line, almost no questions asked besides "what substance?" so we know what antidote to give.
I'm terribly sorry that you have had that experience, and I'm disgusted with people who have treated you that way. However, you are making similar assumptions about me that other people have made about you. Working as an ER tech, I've literally had mental health patients try to strangle me, then given 10 minutes or so to shake it off, and then run straight into another code on a 16 hour shift that did not include any other breaks besides that 10 minutes... and then I came back 8 hours later for another 16 hour shift because the department was so understaffed that it would have been disastrous if I called out sick.
I've come into work, wholly unrecovered from a kidney infection and my own trip to the ER as a patient, and never let a whisper of it show on my face so that I could provide the best care possible for my patients. I've been the patient in the waiting room with 9 out of 10 pain for 6 hours, and I know how much it sucks. That's part of why I do everything I can to give every patient the time, attention, and care that they need to heal them as much as I can.
I'm sorry you had to deal with that awful guy. Abuse of staff isn't something that you should tolerate, nor am I asking you to. All I ask is that patients are not profiled as this guy until they have proven otherwise.
This is a systemic issue, not something that you're expected to fix alone. I'm not blaming you for all the failings of a medical system that is understaffed, underpaid, and overcharged by insurance companies. I'm just asking that people who have suffered at the ER before be heard and believed. I have tried countless times explaining the extent of this systemic issue to medical professionals, and was met with skepticism and outright disbelief about the magnitude of this issue. The many anecdotal experiences from ER visit should give an idea of how common this is among ER visitors.
Yes, it's true that both sides are making assumptions here. However, patient assumptions that ER staff are capable of causing harm are there to keep themselves safe, and don't turn them into abusive patients. Discriminatory assumptions made by ER staff can turn them into abusive staff.
What I have been trying to say is that we didn't make any assumptions about that guy. We treated him with the same standard of care and urgency that any emergent medical condition would warrant until we had proof that he was faking it and after he grabbed a nurse's breast so violently and so hard that the entire right side of her chest was bruised for a couple of weeks. We made no assumptions and only acted on his behaviors and proven medical condition.
The experiences you have had are horrible, but they are not universal. Unfortunately, the way the emergency medical system has been stretched to its limit lately means that the best the ER can do is to keep people from dying, and diagnose and treat the more straightforward conditions. For most of the more complicated and chronic stuff, there's very strict laws about how much medication for what duration can be prescribed by an emergency physician, and a significant amount of the time, the best we can do is make sure you're not actively dying and put in a referral to the specialists with a note that you should be bumped up the waiting list a bit depending on severity. Hell, even trying to admit people to the hospital isn't a sure bet these days because the inpatient departments are allowed to enforce their staffing-to-patient ratios, so the ER gets stuck trying to take care of inpatient and even ICU patients with ER resources for up to days at a time.
My somewhat glib comment about people not being aware of what counts as an "emergency" is very literal when it comes to triage. We do our best to treat everything that comes through our doors, but if there's not an immediate threat to life, limb, or permanent disability, there's pretty distinct limits on what we're able to do on a short timeline and what the hospital allows us to do for free. EMTALA stands for "Emergency Medical Treatment And Labor Act" and it dictates that anyone who turns up to an ER with an emergent medical condition that poses immediate threat to life, limb, or permanent disability will be treated and stabilized to the accepted level of care regardless of ability to pay, and a mother presenting in active labor will be provided with delivery care or appropriate timely transfer to a labor and delivery department if appropriate regardless of ability to pay. There's very strict rules about the level of treatment to be provided and when or if transfer to another facility or provider is warranted and permitted, but past the stipulations of that law, it comes under the hospital administration's rules and regulations about what level of care can be provided by the emergency department.
I've seen quite a few physicians defy the hospital rules by ordering some of the special labs and tests that the specialist would order so that the results are already available in the system for when (if) the patient gets seen by the specialist, but they can get in quite a bit of trouble for it, and if it's not documented just right the patient's insurance might not pay for it. That's one of the other delightful limitations on what the ER can do...we have to toe the line on what needs to or should be done versus what the patient's insurance will pay for, because believe it or not, we really don't want to stick you with a bill for thousands of dollars of tests that your insurance denied coverage for.
Due to overwork, understaffing, antiquated training, and burnout, a lot of physicians' and nurses' bedside manner could use a fair bit of work, but in terms of the care provided, 99+ percent of the time, it really is the best we can do under the restraints created by laws, rules, resources, and insurance.
Permanently disability is exactly what happened to me and so many others when the ER refused to do anything because our pain is not taken seriously. The crux of the issue here is that you cannot 'see' how much pain someone is in and come to a conclusion how pressing their need for medical attention is without further investigation. I'm not asking ER staff to provide treatment beyond what they are supposed to, I'm asking ER staff to provide treatment of what they are supposed to.
The problem is that what constitutes as a medical emergency isn't dictated by patient's pain or symptoms, it's dictated by the medically unsubstantiated biases and preconceptions of medical professionals because patients are presumed drug seeking to be and unreliable witnesses to their own bodies even with clear documentation of prior medical conditions.
Per the laws involved here, "permanent disability" means something like paralysis from a spinal injury, or loss of organ function due to acute critical illness like a necrotic bowel or something. Unfortunately, according to the medical and legal literature on the topic, disability from pain or chronic disease is beyond the required services of an ER. Arguments can be made for acute-on-chronic situations like splenic damage or rupture in sickle cell crisis, but those areas can get pretty fuzzy.
That's a shame. Under disability law, permanent disability is legally defined as a loss of mental or physical function to the point of significantly reducing one's ability to work or perform daily activities for an indefinite period.
It's ironic that medical disability considers the loss of a limb as a permanent disability but not permanent pain and suffering, because I'd gladly trade my leg to know what it's like not to be in pain again and to be treated like a person with a visible disability.
I think you misunderstood. EMTALA defines disability in relation to an emergent condition, injury, or acute illness. The degradation of a chronic condition into a disability is not something that an ER can or should be trying to treat. Disability as a whole can include things like chronic pain in addition to other neuropathies, parasthesias, or paralysis, but the definition of "disability" in terms of emergency medical care is entirely related to the disability being caused by an emergency medical problem, not a chronic one.
I think you are the one misunderstanding here. The medical neglect during my ER visit is what caused my disability. I'm not asking to be treated for chronic pain at the ER, I'm asking to be treated so that I would not have become disabled.
Unless you are obfuscating something, or there were some very unusual mistakes involved, I would think that medical neglect that caused a disability in an acute timeframe would warrant a consultation with a malpractice lawyer.
Medical neglect causing disabilities is much harder to prove than you would think. There is always the benefit of the doubt that doctors are assumed to have tried their best to treat you and that it was a 'coincidence' that you happen to have acquired a chronic condition.
There's nothing unusual about women with abdominal pain being sent home from the ER untreated and berated for coming here 'for no reason'. Women are systemically denied treatment from the ER because every form of abdominal pain is downplayed to being 'just female abdominal pain'. I had severe abdominal pain and spotting when I went to the ER on a Friday evening. I had to wait 4 excruciating hours after an initial screening. Andoctor was finally available and I tried to explain that this wasn't just a normal period and begged to have it checked out, but he doctor wouldn't hear it. He sent me home with ibuprofen and Tylenol and told me not to come back unless it was an emergency.
The OTC meds did jack shit and I already told the doctor I tried ibuprofen before coming. I was left to stew for 3 days, crying, in excruciating pain, and vomiting until I was able to see urgent care on Monday. Those 3 days were the most painful days of my life at the time. At which point I was diagnosed with a hemorrhagic ruptured ovarian cyst through ultrasound that was 3.5 inches in diameter. I was sent in for laparoscopic surgery to remove the cyst. I though that would be the end of it, but that was just the beginning.
I have spoken to my PCP, rheumatologist, and pain therapist about this, and it was universally agreed that the 3 days of neglect and severe pain was a significant contributor to fibromyalgia. Had I been immediately treated, there was a good chance that I may not have ended up permanently in pain. But there is no way to prove it. Any doctor could just say that I would have gotten it anyway.
The ER experience and the pain was beyond traumatizing, but the best part is that this is just the first one. You see, once you have fibromyalgia nothing you ever say in the ER will be believed anymore. The next two times I went to the ER, once for vomiting 24 hours straight and not keeping any fluids down, and once for severe full body pain and a 105F fever, I would be met when even more disdain and disbelief than before. Both times I was told by the advice nurse to go to the ER, and both times I would be eye rolled or reprimanded by at least one person. Keep in mind that I have already had fibromyalgia at this point, and each time I visited the ER it was under severe pain. And each time I regret mentioning fibromyalgia at all because I could immediately tell the change in tone and the insinuations of how I was 'one of those' implying that I am a drug seeker. I had to beg everytime to be treated and to be taken seriously which was immensely difficult to do when I was already delirious from pain.
These people don't know what pain is like with this condition or that how many of us want to kill ourselves because we can't handle the pain and stigma anymore. I'm not telling people about this because I have some personal vendetta, I'm trying to warn people to take everything ER staff say with a grain of salt because ER doctors are human and humans are not immune to implicit biases, and medical misjudgments are often made at the expense of patients who don't fit their preferred demographic.