In October, when the FDA first announced a shortage of Adderall in America, the agency expected it to resolve quickly. But five months in, the effects of the shortage are still making life tough for people with attention-deficit hyperactivity disorder who rely on the drug. Stories abound of frustrated people going to dozens of pharmacies in search of medication each month, only to come up short every time. Without treatment, students have had a hard time in school, and adults have struggled to keep up at work and maintain relationships. The Adderall shortage has ended, but the widely used generic versions of the drug, known as amphetamine mixed salts, are still scarce.
A “perfect storm” of factors—manufacturing delays, labor shortages, tight regulations—is to blame for the shortage, David Goodman, an ADHD expert and a psychiatry professor at the Johns Hopkins University School of Medicine, told me. And they have all been compounded by the fact that the pandemic produced a surge in Americans who want Adderall. The most dramatic changes occurred among adults, according to a recent CDC report on stimulant prescriptions, with increases in some age groups of more than 10 percent in just a single year, from 2020 to 2021. It’s the nature of the spike in demand for Adderall—among adults—that has some ADHD experts worried about “whether the demand is legitimate,” Goodman said. It’s possible that at least some of these new Adderall patients, he said, are getting prescriptions they do not need.
The problem is that America has no standard clinical guidelines for how doctors should diagnose and treat adults with ADHD—a gap the CDC has called a “public health concern.” When people come in wanting help for ADHD, providers have “a lot of choices about what to use and when to use it, and those parameters have implications for good care or bad care,” Craig Surman, a psychiatry professor and an ADHD expert at Harvard and the scientific coordinator of adult-ADHD research at Massachusetts General Hospital, told me. The stimulant shortage will end, but even then, adults with ADHD may not get the care they need.
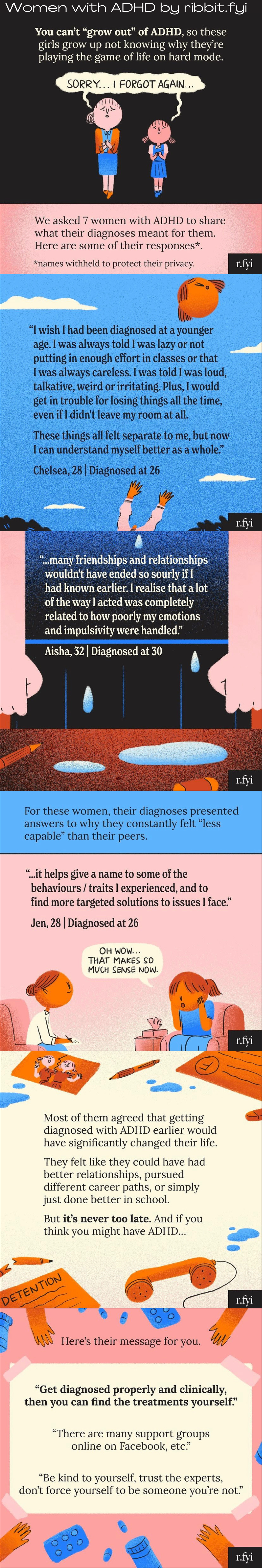
For more than 200 years, symptoms related to ADHD—such as difficulty focusing, inability to sit still, and fidgeting—have largely been associated with children and teenagers. Doctors widely assumed that kids would grow out of it eventually. Although symptoms become “evident at a very early period of life,” one Scottish physician wrote in 1798, “what is very fortunate [is that] it is generally diminished with age.” For some people, ADHD symptoms really do get better as they enter adulthood, but for most, symptoms continue.
The focus on children persists today in part because of parental pressure. Pediatricians have had to build a child-focused ADHD model, Surman said, because parents come in and say, “What are we going to do with our kid?” As a result, treating children ages 4 to 18 for ADHD is relatively straightforward: Clear-cut clinical guidelines from the American Academy of Pediatrics specify the need for rigorous psychiatric testing that rules out other causes and includes reports about the patient from parents and teachers. Treatment usually involves behavior management and, if necessary, medication.
But there is no equivalent playbook for adults with ADHD in the U.S.—unlike in other developed nations, including the U.K. and Canada. In fact, the disorder was only recently acknowledged within the field of adult psychiatry. One reason it went overlooked for so long is because ADHD can sometimes look different in kids compared with adults: Physical hyperactivity tends to decrease with age as opposed to, say, emotional or organizational problems.
“The recognition that ADHD is a life-span disorder that persists into adulthood in most people has really only happened in the last 20 years,” Margaret Sibley, a psychiatry professor at the University of Washington School of Medicine, told me. And the field of adult psychiatry has been slow to catch up. Adult ADHD was directly addressed for the first time in DSM-5—the American Psychiatric Association’s diagnostic bible—in 2013, but the criteria described there still haven’t been translated into practical instructions for clinicians.
Addressing adult ADHD isn’t as simple as adapting children’s standards for grown-ups. A key distinction is that the disorder impairs different aspects of an adult’s life: Whereas a pediatrician would investigate ADHD’s impact at school or at home, a provider evaluating an adult might delve into its effects at work or in romantic relationships. Sources of information differ too: Parents and teachers can shed light on a child’s situation, but “you wouldn’t call the parent of a 40-year-old to get their take on whether the person has ADHD,” Sibley said.
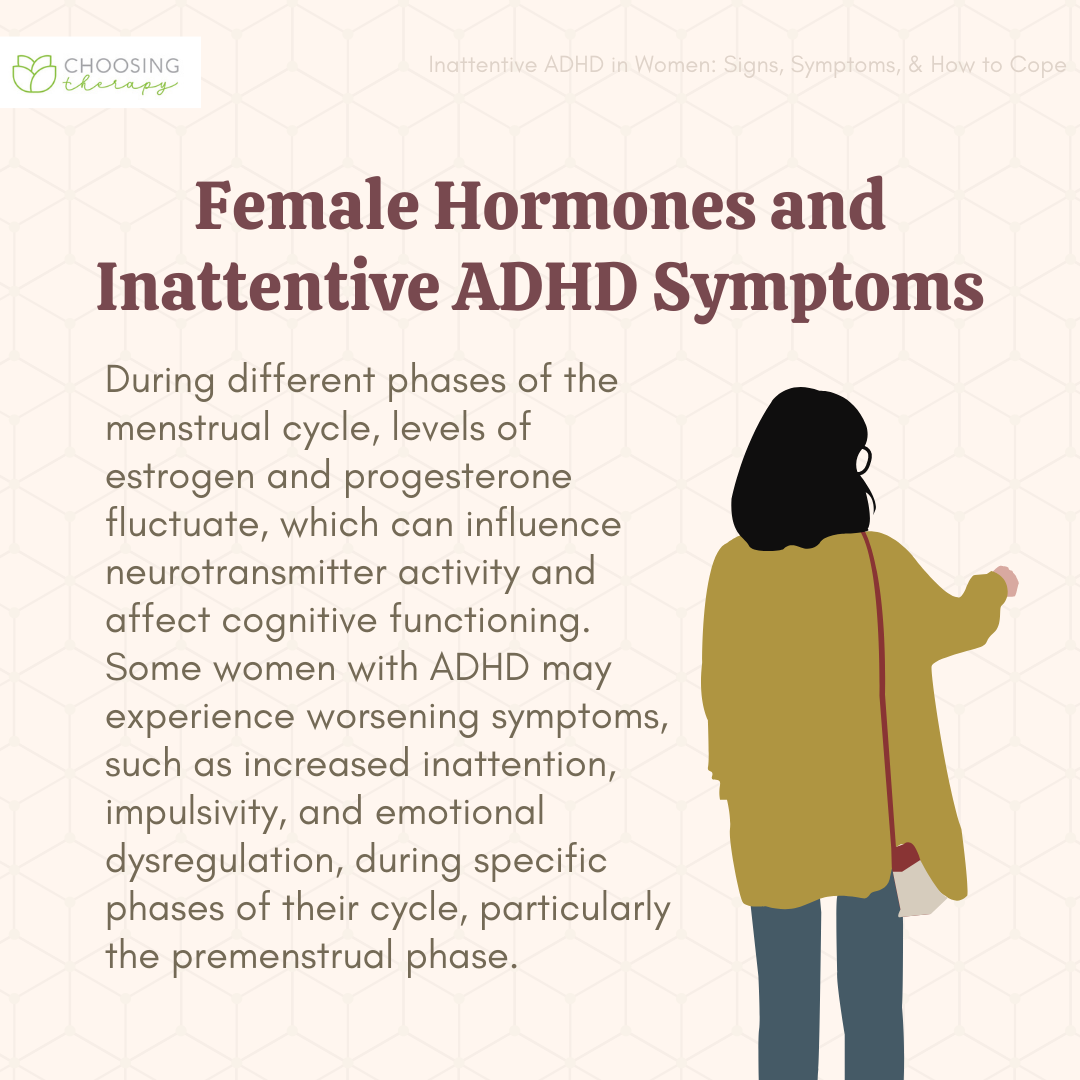
Providers usually rely instead on self-reporting—which isn’t always accurate. Complicating matters, the symptoms of ADHD tend to be masked by other cognitive issues that arise in adulthood, such as those caused by depression, drug use, thyroid problems, or hormonal shifts, Sibley said: “It’s a tough disorder to diagnose, because there’s no objective test.” The best option is to perform a lengthy psychiatric evaluation, which usually involves reviewing symptoms, performing a medical exam, taking the patient’s history, and assessing the patient using rating scales or checklists, according to the APA.
Without clinical guidelines or an organizational body to enforce them, there is no pressure to uphold that standard. Virtual forms of ADHD care that proliferated during the pandemic, for example, were rarely conducive to lengthy evaluations. A major telehealth platform that dispensed ADHD prescriptions, Cerebral, has been investigated for sacrificing medical rigor for speedy treatment and customer satisfaction, potentially letting people without ADHD get Adderall for recreational use.
In one survey, 97 percent of Cerebral users said they’d received a prescription of some kind. Initial consultations with providers lasted just half an hour, reported The Wall Street Journal; former employees feared that the company’s rampant stimulant-prescribing was fueling an addiction crisis. “It’s impossible to do a comprehensive psychiatric evaluation in 30 minutes,” Goodman said. (Cerebral previously denied wrongdoing and no longer prescribes Adderall or other stimulants.)
The bigger problem is that too few providers are equipped to do those evaluations in the first place. Because adult ADHD was only recently recognized, most psychiatrists working today received no formal training in treating the disorder. “There’s a shortage of expertise,” Surman said. “It’s a confusing space where, at this point, consumers often are educating providers.” The dearth of trained professionals means that many adults seeking help for ADHD are seen by providers, including primary-care doctors, social workers, and nurse practitioners, who lack the experience to offer it. “It’s a systemic issue,” Sibley said, “not that they’re being negligent.”
The lack of trained providers opens up the potential for inadequate or even dangerous care. Adderall is just one of many stimulants used to treat ADHD, and choosing the right one for a patient can be challenging—and not all people with ADHD need or want to take them. But even the most well-intentioned health-care professionals may be unprepared to evaluate patients properly. The federal government considers Adderall a highly addictive Schedule II drug, like oxycodone and fentanyl, and the risks of prescribing it unnecessarily are high: Apart from dependency, it can also cause issues such as heart problems, mood changes, anxiety, and depression.
Some people with ADHD might be better off with behavioral therapy or drugs that aren’t stimulants. Unfortunately, it can be all too easy for inexperienced providers to start a patient on these drugs and continue treatment. “If I give stimulants to the average person, they’ll say their mood, their thinking, and their energy are better,” Goodman said. “It’s very important not to make a diagnosis based on the response to stimulant medication.” But the uptick in adults receiving prescriptions for those drugs since at least 2016 is a sign that this might be happening.
The fact that adult ADHD is surging may soon lead to change. Last year, the American Professional Society of ADHD and Related Disorders began drafting the long-needed guidelines. The organization’s goal is to standardize care and treatment for adult ADHD across the country, said Goodman, who is APSARD’s treasurer. Establishing standards could have “broad, sweeping implications” beyond patient care, he added: Their existence could compel more medical schools to teach about adult ADHD, persuade insurance companies to cover treatment, and pressure lawmakers to include it in workplace policies.
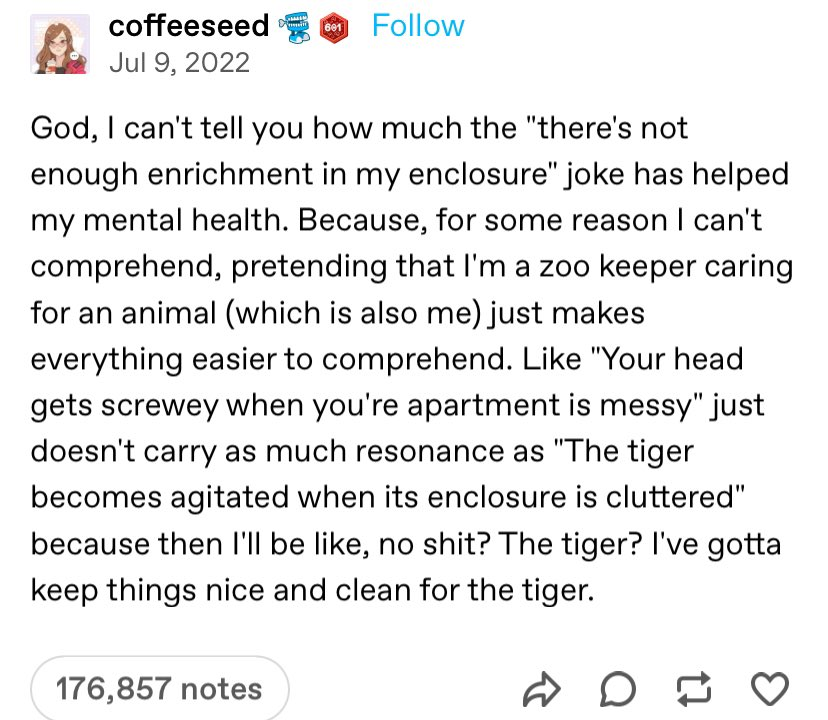
A way out of this mess, however long overdue, is only going to become even more necessary. Nearly 5 percent of adults are thought to have the disorder, but less than 20 percent of them have been diagnosed or have received treatment (compared with about 77 percent of children). “You have a much larger market of recognized and untreated adults, and that will continue to increase,” Goodman said. Women—who, like girls, are historically underdiagnosed—will likely make up a substantial share. Adults with ADHD may have suffered in silence in the past, but a growing awareness of the disorder, made possible by ongoing destigmatization, will continue to boost the ranks of people who want help. On social media, ADHD influencers abound, as do dedicated podcasts on Spotify.
Until guidelines are published—and embedded into medical practice—the adult-ADHD landscape will remain chaotic. Some people will continue to get Adderall prescriptions they don’t need, and others may be unable to get an Adderall prescription they do need. Rules alone couldn’t have prevented the shortage, and they won’t stop it now. But in more ways than one, their absence means that many people who need help for ADHD are unable to receive it.